Boots and all – ankle & feet fracture
Mon,Dec 30, 2019 at 06:39AM by Carla Mullins
Moon-boots are a common sight in my life these days both at work but also on various friends and family members. Post Christmas parties and post new years resolutions are also a time of moon boots. I do wish they were a little bit more fun than the standard black, but I guess they have their purpose of protecting the foot or ankle during a healing phase post a fracture or sprain. As always there are prices to pay for the boot. We ended up running a series on instagram called giving the boot the boot. If you are looking for some videos and simple ideas you can go to the body_organics_education instagram posts from the middle of 2019 there are about 10-15 days of exercises.
In this article we will look at some factors about :
// A reminder of the anatomy of the ankle
// a reminder of fracture and healing considerations for both a fracture and ligament sprain.
// Common fracture of the foot
// What is a Bimalleolar and Trimalleolar fracture (Pott’s fracture)
// Common exercise strategies
// Peripheral sensitisation strategies
A refresher of the anatomy of the ankle?
The bones that form the ankle are essentially:
// Tibia
// Fibular
// Talus
// Calcaneus
The Talus is a dome shaped, and oddly enough has no muscles attaching to it. The Fibular (sits on the outside) and the Tibia ( on the inside) both have small protrusion of bone that sit either side of the Talus almost like a clamp ( this is called the Mortise).
When we bend the knee our Tibia and Fibular slide forward at the ankle and the Talus glides backwards. As the Tibia and Fibular move they pivot on each other, a bit like saloon doors swing around each other. Accordingly, when we move there are rhythms happening with the bones, and a fracture and subsequent immobility interfere with those rhythms. As a result we see collateral damage in knees, hips and sacrum, as discussed later in this article.
Remember also that ligaments are how we stabilise the joints, and they can easily be stretched or sprained. The foot and ankle have many bones and therefore many ligaments. The most common ligaments of the ankle that are damaged are:
// Deltoid ligament is injured with pronation (eversion) trauma leading to forced external rotation and abduction of ankle. This is called a high ankle sprain, This often occurs in football tackles
// Calcaneal fibular ligament ( on the outside/lateral side of the foot) – often injured when the foot is inverted in dorsi flexion and inverts. When injured it is called a low ankle sprain
// Lateral Talocalcaneal Ligament (LTCL)
// Anterior Talofibular Ligament (ATFL)
// Posterior Talofibular Ligament (PTFL) this is rarely injured and when it does it is associated wiht fracture and dislocation of the Tibia.
There are three grades of ligament sprain:
// Grade 1: Over stretching of the ligaments, tearing of only a few fibres. there will be pain but minimal swelling or bruising.
// Grade 2: This includes a tear ranging from part of the ligament to most of the ligament. There will be moderate to severe pain and often swelling and bruising as well. If a person has experienced a significant grade 2 ligament sprain they will be in a moon boot for approximately 6-8 weeks.
// Grade 3: This is a complete tear of the ligament. Often, there will be pain initially but it will subside quickly as the nervous structure has also been compromised. There will be pain and swelling and this will cause pain to surrounding nerves and structures. If a person has experienced a grade 3 ligament sprain they will be in a moon boot for approximately 6 – 8 weeks.
It is important to remember that each time a person sprains an ankle they increase the likelihood of re-spraining the ankle. Accordingly, it is important to focus on strengthening supporting muscles to help stabilise the ankle. It is also important to work on ways to help the person improve proprioceptive awareness of the ankle to reduce clumsiness. Remember with proprioception the receptors are in the joint, tendon and muscle but the process is generally neurological happening in your brain. Taking the time to train proprioception is important and for those interested we cover it in the Body Organics Chucking a Wobbly course (Australia and USA) and in the online Anatomy Dimensions feet course
What is a fracture; and healing considerations?
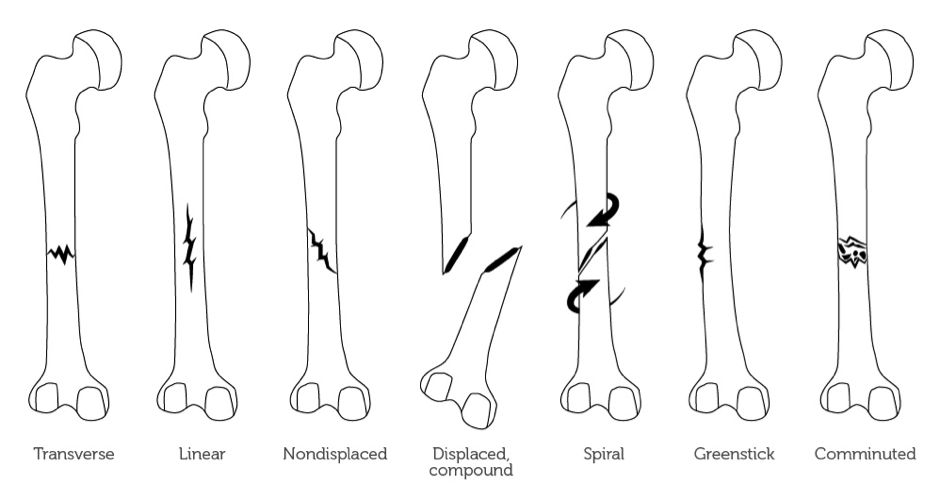
When it comes to fractures of any bones it is always important to know the type of fracture with which you are dealing. Below are basic definitions of the different fracture types:
//Transverse: The bone is broken in two, with the fragments remaining in place.
//Spiral: The line of force is at an oblique or a rotational force line that has been applied, resulting in the fracture.
//Comminuted: There is more than one fragment of bone, which can also be referred to as a segmental fracture.
//Greenstick: The bone is buckled or bent.
//Compression: The cancellous bone is crumpled.
//Avulsion: Where a fragment of bone has been torn away from the main bone by a ligament or tendon.
When dealing with fractures it is important to know whether or not the fracture is displaced or non- displaced. In other words, has the bone moved significantly apart and therefore needs to be pinned back together? It is also important to understand whether the bone is at risk of becoming displaced if there is any weight bearing, which is particularly relevant to pelvic and lower limb fractures. Weight bearing too early can result in a slight displacement and mal-union of the bones, hence moon boots and casts.
Fracture healing
Healing of bone occurs in five stages:
1. Tissue death and haematoma formation: Vessels are torn and a haematoma forms around and within the fracture. Bone tissue dies, 1-2mm of cellular death on either side of the fracture (48 hours from fracture).
2. Inflammation and cellular proliferation: Acute inflammatory reaction under the periosteum and within the breached medullary canal. Fracture ends are surrounded by cellular tissue, forming bridges and allowing for capillary growth (first 1-2 weeks).
3. Callus formation: The proliferating cells are chondrogenic and osteogenic. Under the right conditions, bone with cartilage forms. Osteoclasts commence mopping up dead bone. The immature group of cells forms a callus/splint on the periosteal and endosteal surfaces (2-3 weeks).
4. Consolidation: With continuing osteoclast and osteoblastic activity, the woven bone is transformed into lamellar bone. The system is now rigid enough to bear normal loads (6-12 week stage).
5. Remodelling: The fracture has been bridged by a cuff of solid bone, which will form over a period of months. Following formation of solid bone, which may take years, there will be continued reformation/absorption of bone and adaptation in order to reinforce areas of high load (12 months plus).
The periods of time mentioned above for bone healing is indicative only and can vary depending on a person’s health, diet and age. Smoking will delay the healing process, as well poor overall health and poor nutrition.
What are types of fractures associated with the foot and ankle?
The common fractures of the foot which require a moon boot include:
// Lisfranc fracture – one or all of the metatarsals are displaced from the tarsus
// Jones fracture – a fracture of the fifth metatarsal base/zone
// March fracture – a fracture of the distal third of one of the metatarsals occurring because of recurrent stress
The common fractures of the Ankle include:
// Bimalleolar fracture (medial and lateral malleolus) and
// Trimalleolar (bimalleolar plus the distal posterior aspect of tibia– posterior malleolus)
All of these fractures are associated with significant ligament damage and often dislocation of the ankle mortise, which is essentially the Tibia as it sits over the Talus.
MRIs and x-rays are required to determine the location and degree of fractures in order to formulate surgical or conservative treatment plans. In many cases as both tibial and fibula integrity has been lost with concomitant disruption of the syndesmosis unit and medial/lateral ligament complex, and surgery is always required. This is the case if there are any displaced or large fractures in the medial/lateral/posterior malleolus or any fracture involving the ankle mortise. In the case of smaller non-displaced fractures not involving the ankle mortise a casting or moon boot orthoses and crutches may be implemented to manage conservatively. Length of time non weight bearing and immobilised can vary on the degree of fracture.
Following surgery or cast removal rehabilitation on the ankle and foot complex should commence to:
// restore range,
// intrinsic and extrinsic strength and
// balance/proprioception (as post op protocol allows).
Orthoses and footwear modification can assist in return of function and rehabilitation once weight bearing has commenced.
Fractures
It’s important to remember the stages of healing of a fracture when you are dealing with clients.
Fracture Healing Healing occurs in five stages:
1. Tissue death and haematoma formation: vessels are torn and a haematoma forms around and within the fracture. Bone tissue dies, 1-2mm of cellular death on either side of the fracture. This lasts for around 24 to 48 hours.
2. Inflammation and cellular proliferation: acute inflammatory reaction under the periosteum and within the breached medullary canal. Fracture ends are surrounded by cellular tissue forming bridges, allowing for capillary growth. This takes around 7 to 14 days post injury.
3. Callus formation: the proliferating cells are chondrogenic and osteogenic. Under the right conditions, bone with cartilage forms. Osteoclasts commence mopping up dead bone. The immature group of cells forms a callus/splint on the periosteal and endosteal surfaces. This happens for up to 6-8 weeks post injury.
4. Consolidation: with continuing osteoclast and osteoblastic activity, the woven bone is transformed into lamellar bone. The system is now rigid enough to bear normal loads. This should be achieved around 6- 8 weeks post injury and is when you get to stop wearing the moon boot.
5. Remodelling: the fracture has been bridged by a cuff of solid bone which will form over a period of months. Following formation of solid bone, which may take years, there will be continued reformation/absorption of bone and adaptation in order to reinforce areas of high load.
Remember, the healing process is the healing process and cannot be rushed.
Exercise strategies for specific sporting injuries
// Understanding the state of the human body (structural) and a person’s profile. This cannot be established on a single visit, but can be determined over a period of time. Pilates teachers are in a good position to understand this because generally we have been working with our clients for some time and they are coming in with this fracture and are trusting us to understand how to keep them working without aggravating the foot or the healing process
// Timing – when to initiate or reduce or increase a person’s exercise program. Achieving realistic time frames/ expectations.
// Knowing when to treat and when to refer.
// Communicating with the patient/client about yours and their expectations.
// Person’s exercise history – coming from another sport and trying another?
-
No loading history?
-
Elite athlete?
-
Post surgical?
-
Chronic medical condition (e.g. lower back?)
// Influence of the lower limb on higher order structures is significant. Do not underestimate how poor foot and ankle posture and the effect on hips and knees. The number of times that I have seen a person limping around in a moon boot, loading up their SIJ , knee joints and the opposite ankle. When I see clients with a moon boot on to protect their foot, i know we have to work on releasing their pelvis and getting them moving and releasing their lower spine whilst also stabilising the pelvis for the additional walking.
Introduction of weight-bearing
Having not weight borne on the affected side for nearly eight weeks, there will be some issues when the person does have to stand on both feet. the first problem is that the non-weight bearing foot can acquire peripheral sensitivity, as it had lost a lot of its sensory memory from having no pressure on the foot. The result was a lot of pins and needle type pain as the person starts walking around, and very little tolerance for pressure on his feet for a few weeks. It is important to ensure that your client is undertaking peripheral sensitisation work throughout the process and had given him some exercises to help mitigate the pain.
What is peripheral sensitivity?
In simple terms, our body receives sensation and feedback through our skin and that creates a feedback loop in our brain. When we don’t use a part of our body for a while the feedback loop becomes dulled and we start to get mixed messages from our sensory input system. Something that is normally just an easy movement can start to feel extremely painful – this is the central pain sensitivity we hear about. It is for this reason that it is important that people expose their receptors to sensory input when the body parts aren’t being used because of trauma or damage. In situations where a person is in a non-weight bearing boot, it is important to ensure that feet are exposed to different sensations, e.g. fabrics, textures so that he could keep the sensory pathways working. Scrunching a towel with a foot was also advised provided it does not aggravate the underlying fracture. In some people this sensitivity can escalate into quite chronic pain problems.
I have been particularly aware of this issue when Max (my then four year old son) had fallen off some monkey bars and broken his arm and his father Michael fell off his bicycle and broke his pelvis (yes, a very accident-prone family!). Not surprisingly Max did not take well to following the surgeon’s advice of just keeping his arm in a sling and not moving it for 6-8 weeks. So I took him to an occupational therapist and had a special removable cast made for the elbow, then he could still use his hands and the skin around his affected area could feel the water and other sensations. The result is that he was still able to use his hands and did not end up with any sensory issues, particularly as this injury occurred before he was six years old and therefore at a point when important sensory planning and memory systems were being laid down in his brain.
What does peripheral sensitivity mean for your clients?
If you have clients wearing a moon boot or a cast, e.g. because of a foot fracture, then it is important that you work with a physiotherapist or occupational therapist, if possible, to get ideas on how to incorporate sensitisation strategies in the studio setting. Here are some simple ideas:
// Use different textured fabrics and rub them or slide them across the affected area.
// use Markarlu Lotus for sensitisation exercises. The Makarlu Beach ( is a nesting tool similar to Markalu Lotus but with different textures). Makarlu beach is to be launched in 2020 and has a number of additional variations and textures embedded within it to aid with peripheral sensitivity and neuropathy exercises, and this article will be updated to incorporate those ideas when Makarlu Beach is launched.// Try marbles, sand, pebbles, theraputty or play dough to help keep the sensory pathways functioning.
// Vary the water temperature to have the person feel cold water, lukewarm water etc.// In the studio setting you could have the person, for example, resting their feet on different fabrics throughout the class.
to buy makarlu lotus you can purchase from
Shop Makarlu
makarlu coast will be available in 2021 .
If you are located in Brisbane our Physiotherapists, Podiatrists, Acupuncturists, Naturopaths and pilates teachers are available to work with you to help you through the process of healing and recovery,
To find out more about lower limb fractures and processes for recovery and strategies that can be incorporated into a studio or home setting try our professionally filmed and edited online Anatomy Dimensions courses
For more information about our products, online and face to face courses email us education@bodyorganics.com.au or look at our education courses list

 0
0