Spondylolisthesis and spondylolysis – causes, symptoms and exercises
Mon,May 15, 2017 at 01:20PM by Carla Mullins
Spondylolisthesis and spondylolysis are terms that strike fear into the hearts of many, even if it’s only how to pronounce the words or to spell them. However, the conditions are common and manageable if the person seeks treatment and complies with their exercise program. My own mother at the age of 77 started complaining of intense pain in her back, only to find out that a stress fracture she was unaware of for many years (spondylolysis) had become spondylolisthesis, so all of a sudden she was in severe pain.
In this article we will be covering:
// What are spondylolisthesis and spondylolysis;
// Some of the common causes and situations;
// What are the common treatments for these conditions;
// What are the common contraindications;
// Some considerations for exercise;
// Some simple ways to modify pilates exercises for people with this condition.
Note that this article is part of the work we cover in more detail in the Diploma of Pilates Movement Therapy NAT 10567 and the Anatomy Dimensions Spine and Torso workshops.
What is spondylolisthesis?
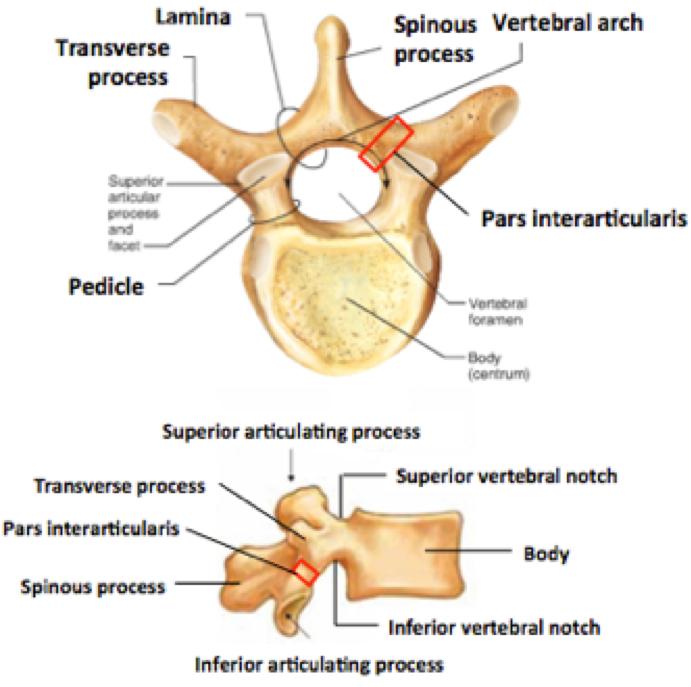
The term spondylolisthesis describes a condition in which a vertebra in the spine slips on the vertebra below. The vertebra most commonly slips anteriorly (anterolisthesis), but may also slip posteriorly (retrolisthesis). The slippage is associated with a bilateral deficit in the pars interarticularis (see the picture below) and is most common between L5 and S1, however also commonly occurs between L4 and L5. A pars fracture can occur without any slippage of the vertebrae and this is then known as spondylolysis. A spondylolysis is quite common occurrence in children as young as 7 years, often due to repetitive sports loading, e.g. gymnastics.
Remember that spondylolisthesis can occur in children and teenagers who can have difficulty explaining why they are in pain, or more commonly having people properly listen to them. As one parent recently explained:
“No one would listen to my ten year old daughter when she said she was in pain and was told to just ‘toughen up’. When she was finally treated and diagnosed she was in a lot of pain and her condition had been aggravated by exercises such as swimming (note: due to extension of the legs and lower back). Teachers at school would only stop pushing her in sports once X rays had been taken”
This mother’s advice was listen to kids when they are in pain and get it investigated as soon as possible.
There are a number of different reasons why a spondylolisthesis can occur:
// In children it is often due to a birth defect in that area of the spine;
// Due to a lesion in the pars interarticularis, such as an acute traumatic fracture, or repetitive micro-fractures resulting in elongation of the pars;
// Degenerative spondylolisthesis due to degeneration of structures such as the facet joints or discs;
// Due to an acute trauma leading to fracture in parts of the spine other than the pars interarticularis;
// Post-surgery where too much of the posterior spinal structures have been removed;
// Due to some diseases/pathologies such as spina bifida, Scheuermann’s disease, spinal stenosis, etc;
// Certain sporting activities such as gymnastics, weight lifting, football and fast bowling in cricket can put a great deal of stress on the bones in the lower back. They also require that the athletes constantly overstretch (hyperextend) the spine. This can lead to a stress fracture of the pars interarticularis on one or both sides of the vertebra.
The existence of a spondylolisthesis does not always result in pain, particularly if it is only a low-grade slippage.
Spondylolisthesis is graded as follows:
Grade 1 – the top vertebra has slipped up to 25% over the body of the vertebra below.
Grade 2 – the top vertebra has slipped between 25-50%.
Grade 3 – the top vertebra has slipped between 50-75%
Grade 4 – the top vertebra has slipped over 75%.
What are the symptoms of spondylolisthesis?
Spondylolisthesis may be asymptomatic, however some symptoms include:
// Low back pain – usually worse standing rather than sitting, if they sleep on their stomach, after exercise or with lumbar extension;
// Dull ache and/or numbness or weakness in the buttock or posterior thigh;
// Tight hamstrings, as the body tries to protect the lumbar spine by limiting the lordosis;
// Reduced ability to control their bladder or bowel;
// In severe cases the gait pattern is changed so that you see more of a waddling style of walking with their abdomen protruding.
It is important to note that people with spondylolisthesis will often develop a hyper-lordosis. This postural pattern allows them to transfer the weight-bearing load from the vertebral bodies onto the facet joints of the spine. A further compensatory pattern is to then develop lordotic-kyphotic posture.
This educational animated video from Dr. Nabil Ebraheim describes the difference between spondylolysis, spondylolisthesis, spondylitis and spondylosis. It includes a useful image of what happens when there is a spondylolisthesis that can be helpful when discussing the condition with your clients.
What are some concerning neurological symptoms?
It is important to make sure that the client is seen immediately by a medical practitioner if they are presenting with:
// Shooting pains, burning, numbness, pins and needles, weakness or paralysis;
// Cauda equina syndrome symptoms (this is a medical emergency). Symptoms include: bilateral shooting pains down the backs of the legs, saddle region anesthesia, loss of bowel and bladder control, bilateral foot weakness, quadriceps weakness, and severe back pain. The sacral nerve roots are compressed as they pass through the spinal canal as affected by the spondylolisthesis.
What are some exercise precautions and contra-indications for spondylolysis and spondylolisthesis?
The exercise precautions for this are generally to be careful or avoid lumbar extension and to encourage greater lumbar flexion. It is also very important to work on improving lumbopelvic stability. Remember that with this condition if the vertebra is stable and there is no pain, then you need to ensure that you optimise spinal movement elsewhere in the spine. Just because the person should not experience lumbar extension at one level does not mean the rest of the spine cannot have optimal range of movement. You just need to be careful in how you do this.
Extension of the lumbar spine will increase the pressure in the area and if the injury is spondylolysis it may considerably increase pain. If it is a spondylolisthesis then extension may aggravate the slippage and instability that is already present (dependant on the cause of the spondylolisthesis); thus these movements should be avoided. Flexion of the spine will distract the posterior surfaces of the vertebra away from each other, as well as stretch the lower back musculature that is most likely in spasm so lumbar flexion should be encouraged. The slippage of the spondylolisthesis may also cause narrowing of the spinal canal, which is another reason that spinal flexion is indicated. In the acute stage single legwork may aggravate symptoms.
What should you do with someone that has a spondylolysis or a spondylolisthesis?
Improving muscle strength in the torso is important, as is balance. Look to reduce extension forces on the spine potentially by improving abdominal muscle strength and lengthening the spinal extensors, which may be tight.
1. Stretch hamstrings
Hamstrings tend to spasm in people with low back pain. This will increase the tension of the posterior fascial system and can aggravate the pain. Gently move your clients into a comfortable stretch, i.e. don’t over stretch! Focus on reaching the sit-bones away while maintaining a neutral spine.
2. Stretch and release the gluteal muscles
Once again the gluteal muscles tend to spasm to protect the low back when there is instability. Unfortunately, instead of stabilising the area it increases the strain on the fascia that inserts on the lower back, aggravating symptoms. Gluteal release can be very effective and also encourages the core to activate. Be careful when stretching the glutes to avoid extension and rotation in the lower back. Try to keep as much of a neutral spine as possible.
3. Strengthen deep postural muscles
When back injuries occur the superficial muscles such as the paraspinal and the quadratus lumborum tend to spasm to “brace” the back. This has many implications on the localised stabilising muscles. Because the superficial muscles are doing more than their share of work, the deep stabilising muscles such as the transversus abdominis, pelvic floor and multifidus don’t have the same load that they usually do, so they take a break and turn off. Clinically we refer to this as inhibition of the “deep core muscles”.
This can become a very dangerous downward spiral and what we see clinically is this:
// Clients back is in spasm and the stabilising muscles are inhibited;
// Back spasm starts to ease and client feels a bit better, but stability has been compromised;
// Client does x-y movement and the back realises that it does not have appropriate stability to achieve a “normal“ range of movement;
// Back spasms again and the cycle is repeated. To break the cycle you have to teach the client to activate their deep postural muscles when stability is required during loaded work.
4. Strengthen multifidus and back extensor muscles
It is important to differentiate spasm and tight back muscles from strong back muscles. It is the voluntary contractile properties of muscle that define it as strong or weak. This is often seen in back pain, the involuntary spasm of the back that makes it look like the muscles are strong is actually weakening the contractile properties of the muscle. Once the muscle spasm has decreased, the back extensor muscles and deep core muscles need to be strengthened, slowly and carefully. Ensure that core is always activated and there is a lengthening through the sacrum when working towards lumbar extension. This will help to decrease the load on the vertebra.
5. Reinforce posture and pelvic alignment
Work on pelvic alignment in sitting, standing, supine and four point to reinforce the importance of posture in spinal health.
What are some contraindicated exercises?
// No prone work without pillow or towel under the stomach or pelvis;
// No lumbar extension but thoracic extension is fine;
// Care with hip extension as poor mechanics can result in the pelvis being moved into an anterior tilt at the end of range hip extension.
Some ideas for exercise and modifications

4PointKneeling on the mat can be modified so that the person’s lumbar spine is supported by a box so as to block the pull of gravity. Discussed in detail in the mat and movement manual

Prone on the Spine corrector

Supported towel C curve (from our Prepilates Supine manual)

Hoof on the CoreAlign or Reformer (from our CoreAlign One or Reformer Three manuals)

Hoof with flexion on the CoreAlign (from our CoreAlign One or Reformer Three manuals)

Genie on the High Barrel (from our Barrel and Arc manual)

Seated stick exercises



Glute release using the Makarlu
In this video we look at some ideas to help with unlocking a lumbar spine and achieving hamstring, psoas and glute balance.
Other examples and modifications can be found throughout the Body Organics Repertoire Manuals which detail the teaching points, contraindications and modifications for conditions such as spondylolisthesis. This topic is explored in more depth as part of our Foundational Workshops sereis Anatomy Dimensions spine and torso courses, This course is availbale online and when possible we offer these courses in person. All course participants receive high quality colour manuals, detailed instruction and valuable information about pathologies and how to adjust, modify and teach for pathologies. Our courses are designed to help practitioners who don’t always have healthy clients .
 0
0